Medical devices – the wild west for cybersecurity vulnerabilities and savvy hackers
 Medical devices are incredibly vulnerable to hacking attacks. In some cases it’s because of software defects that allow for exploits, like buffer overflows, SQL injection or insecure direct object references. In other cases, you can blame misconfigurations, lack of encryption (or weak encryption), non-secure data/control networks, unfettered wireless access, and worse.
Medical devices are incredibly vulnerable to hacking attacks. In some cases it’s because of software defects that allow for exploits, like buffer overflows, SQL injection or insecure direct object references. In other cases, you can blame misconfigurations, lack of encryption (or weak encryption), non-secure data/control networks, unfettered wireless access, and worse.
Why would hackers go after medical devices? Lots of reasons. To name but one: It’s a potential terrorist threat against real human beings. Remember that Dick Cheney famously disabled the wireless capabilities of his implanted heart monitor for fear of an assassination attack.
Certainly healthcare organizations are being targeted for everything from theft of medical records to ransomware. To quote the report “Hacking Healthcare IT in 2016,” from the Institute for Critical Infrastructure Technology (ICIT):
The Healthcare sector manages very sensitive and diverse data, which ranges from personal identifiable information (PII) to financial information. Data is increasingly stored digitally as electronic Protected Health Information (ePHI). Systems belonging to the Healthcare sector and the Federal Government have recently been targeted because they contain vast amounts of PII and financial data. Both sectors collect, store, and protect data concerning United States citizens and government employees. The government systems are considered more difficult to attack because the United States Government has been investing in cybersecurity for a (slightly) longer period. Healthcare systems attract more attackers because they contain a wider variety of information. An electronic health record (EHR) contains a patient’s personal identifiable information, their private health information, and their financial information.
EHR adoption has increased over the past few years under the Health Information Technology and Economics Clinical Health (HITECH) Act. Stan Wisseman [from Hewlett-Packard] comments, “EHRs enable greater access to patient records and facilitate sharing of information among providers, payers and patients themselves. However, with extensive access, more centralized data storage, and confidential information sent over networks, there is an increased risk of privacy breach through data leakage, theft, loss, or cyber-attack. A cautious approach to IT integration is warranted to ensure that patients’ sensitive information is protected.”
Let’s talk devices. Those could be everything from emergency-room monitors to pacemakers to insulin pumps to X-ray machines whose radiation settings might be changed or overridden by malware. The ICIT report says,
Mobile devices introduce new threat vectors to the organization. Employees and patients expand the attack surface by connecting smartphones, tablets, and computers to the network. Healthcare organizations can address the pervasiveness of mobile devices through an Acceptable Use policy and a Bring-Your-Own-Device policy. Acceptable Use policies govern what data can be accessed on what devices. BYOD policies benefit healthcare organizations by decreasing the cost of infrastructure and by increasing employee productivity. Mobile devices can be corrupted, lost, or stolen. The BYOD policy should address how the information security team will mitigate the risk of compromised devices. One solution is to install software to remotely wipe devices upon command or if they do not reconnect to the network after a fixed period. Another solution is to have mobile devices connect from a secured virtual private network to a virtual environment. The virtual machine should have data loss prevention software that restricts whether data can be accessed or transferred out of the environment.
The Internet of Things – and the increased prevalence of medical devices connected hospital or home networks – increase the risk. What can you do about it? The ICIT report says,
The best mitigation strategy to ensure trust in a network connected to the internet of things, and to mitigate future cyber events in general, begins with knowing what devices are connected to the network, why those devices are connected to the network, and how those devices are individually configured. Otherwise, attackers can conduct old and innovative attacks without the organization’s knowledge by compromising that one insecure system.
Given how common these devices are, keeping IT in the loop may seem impossible — but we must rise to the challenge, ICIT says:
If a cyber network is a castle, then every insecure device with a connection to the internet is a secret passage that the adversary can exploit to infiltrate the network. Security systems are reactive. They have to know about something before they can recognize it. Modern systems already have difficulty preventing intrusion by slight variations of known malware. Most commercial security solutions such as firewalls, IDS/ IPS, and behavioral analytic systems function by monitoring where the attacker could attack the network and protecting those weakened points. The tools cannot protect systems that IT and the information security team are not aware exist.
The home environment – or any use outside the hospital setting – is another huge concern, says the report:
Remote monitoring devices could enable attackers to track the activity and health information of individuals over time. This possibility could impose a chilling effect on some patients. While the effect may lessen over time as remote monitoring technologies become normal, it could alter patient behavior enough to cause alarm and panic.
Pain medicine pumps and other devices that distribute controlled substances are likely high value targets to some attackers. If compromise of a system is as simple as downloading free malware to a USB and plugging the USB into the pump, then average drug addicts can exploit homecare and other vulnerable patients by fooling the monitors. One of the simpler mitigation strategies would be to combine remote monitoring technologies with sensors that aggregate activity data to match a profile of expected user activity.
A major responsibility falls onto the device makers – and the programmers who create the embedded software. For the most part, they are simply not up to the challenge of designing secure devices, and may not have the polices, practices and tools in place to get cybersecurity right. Regrettably, the ICIT report doesn’t go into much detail about the embedded software, but does state,
Unlike cell phones and other trendy technologies, embedded devices require years of research and development; sadly, cybersecurity is a new concept to many healthcare manufacturers and it may be years before the next generation of embedded devices incorporates security into its architecture. In other sectors, if a vulnerability is discovered, then developers rush to create and issue a patch. In the healthcare and embedded device environment, this approach is infeasible. Developers must anticipate what the cyber landscape will look like years in advance if they hope to preempt attacks on their devices. This model is unattainable.
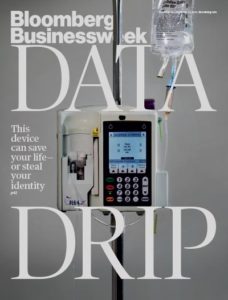
In November 2015, Bloomberg Businessweek published a chilling story, “It’s Way too Easy to Hack the Hospital.” The authors, Monte Reel and Jordon Robertson, wrote about one hacker, Billy Rios:
Shortly after flying home from the Mayo gig, Rios ordered his first device—a Hospira Symbiq infusion pump. He wasn’t targeting that particular manufacturer or model to investigate; he simply happened to find one posted on EBay for about $100. It was an odd feeling, putting it in his online shopping cart. Was buying one of these without some sort of license even legal? he wondered. Is it OK to crack this open?
Infusion pumps can be found in almost every hospital room, usually affixed to a metal stand next to the patient’s bed, automatically delivering intravenous drips, injectable drugs, or other fluids into a patient’s bloodstream. Hospira, a company that was bought by Pfizer this year, is a leading manufacturer of the devices, with several different models on the market. On the company’s website, an article explains that “smart pumps” are designed to improve patient safety by automating intravenous drug delivery, which it says accounts for 56 percent of all medication errors.
Rios connected his pump to a computer network, just as a hospital would, and discovered it was possible to remotely take over the machine and “press” the buttons on the device’s touchscreen, as if someone were standing right in front of it. He found that he could set the machine to dump an entire vial of medication into a patient. A doctor or nurse standing in front of the machine might be able to spot such a manipulation and stop the infusion before the entire vial empties, but a hospital staff member keeping an eye on the pump from a centralized monitoring station wouldn’t notice a thing, he says.
The 97-page ICIT report makes some recommendations, which I heartily agree with.
- With each item connected to the internet of things there is a universe of vulnerabilities. Empirical evidence of aggressive penetration testing before and after a medical device is released to the public must be a manufacturer requirement.
- Ongoing training must be paramount in any responsible healthcare organization. Adversarial initiatives typically start with targeting staff via spear phishing and watering hole attacks. The act of an ill- prepared executive clicking on a malicious link can trigger a hurricane of immediate and long term negative impact on the organization and innocent individuals whose records were exfiltrated or manipulated by bad actors.
- A cybersecurity-centric culture must demand safer devices from manufacturers, privacy adherence by the healthcare sector as a whole and legislation that expedites the path to a more secure and technologically scalable future by policy makers.
This whole thing is scary. The healthcare industry needs to set up its game on cybersecurity.